Groundbreaking research reveals a hidden bias in how a potentially deadly heart condition is diagnosed, putting women at risk of being overlooked. Prepare to have your assumptions challenged.
Unveiling the Hidden Bias
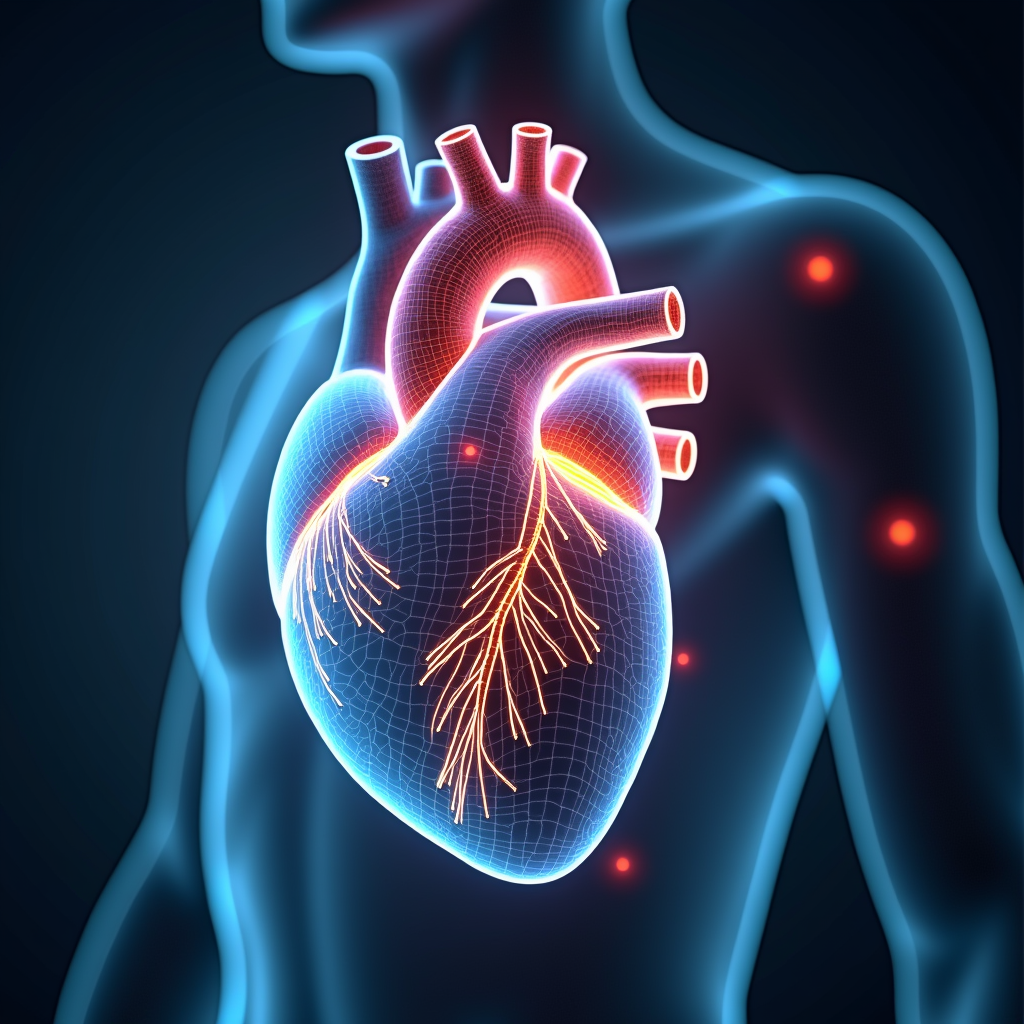
For decades, guidelines for diagnosing hypertrophic cardiomyopathy (HCM) – a genetic condition causing thickened heart muscles – have relied on a one-size-fits-all approach. However, new research led by UCL scientists exposes a concerning flaw: this outdated method fails to account for natural differences in sex and body size, resulting in a striking gender disparity. Typically, two-thirds of HCM diagnoses are given to men, despite the condition being equally likely in women.

A Breakthrough in Personalized Diagnosis?
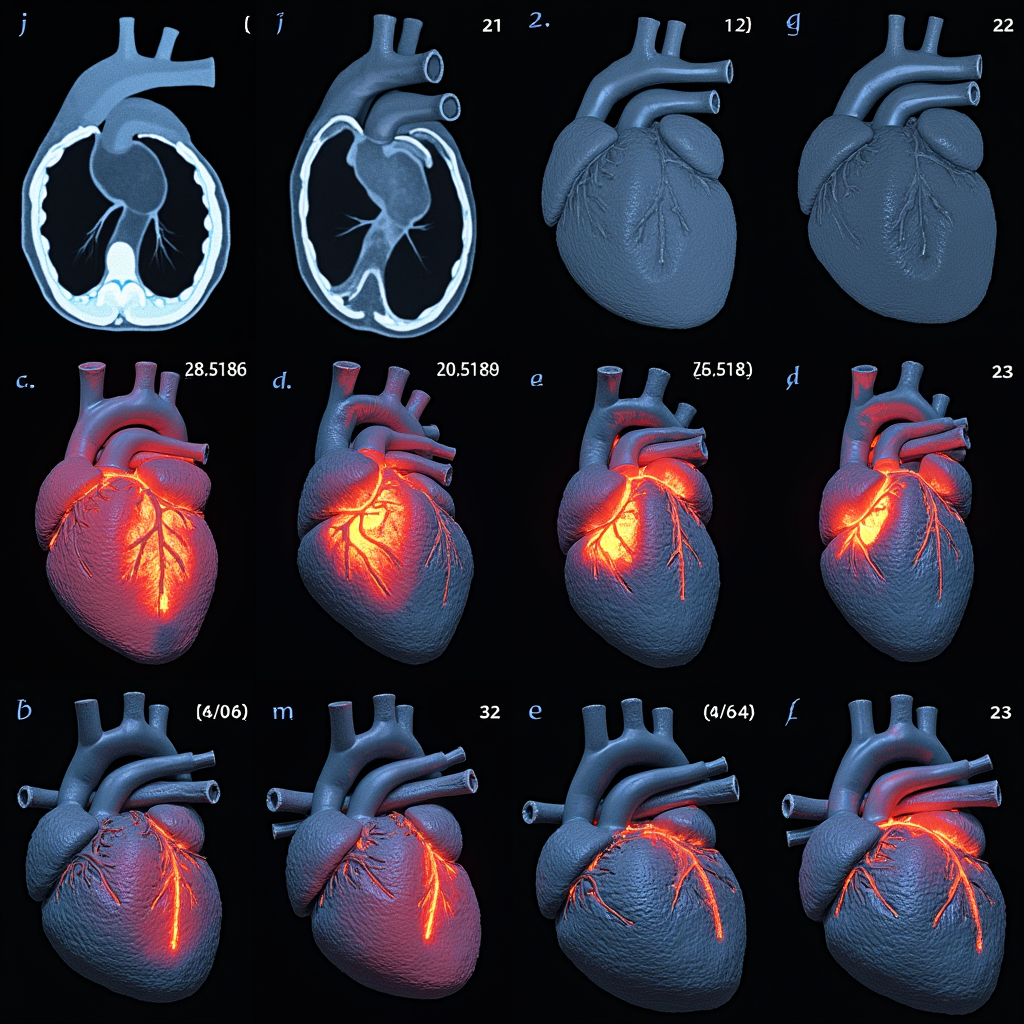
In a groundbreaking study, researchers developed an AI tool to precisely analyze over 5,000 MRI scans of healthy hearts. By measuring the thickness of the left ventricle wall, they uncovered that ‘normal’ thickness varies based on age, sex, and body surface area. This revelation paved the way for a personalized approach to defining abnormal heart wall thickness – a key indicator of HCM.
The AI-Powered Solution
Armed with this newfound understanding, the team tested their AI-driven method on 1,600 patients clinically diagnosed with HCM. The results were striking: by accounting for individual factors like sex and size, the personalized thresholds identified 20% more women with the condition compared to the outdated guidelines. This suggests that countless women may have been missed by the previous one-size-fits-all criteria.

Redefining ‘Abnormal’ for Accurate Detection
But the implications don’t stop there. When applied to over 43,000 participants in the UK Biobank, the personalized thresholds not only identified more women but also reduced the overall number of potential HCM cases. This hints at a reduction in misdiagnoses, ensuring that those truly affected receive the care they need without unnecessarily alarming others.
Closing the Diagnostic Divide
Dr. Hunain Shiwani, the study’s lead author, emphasizes the urgency of reconsidering the current guidelines: ‘It is clear that this threshold, which is based on the results of studies from the 1970s, needs to be reconsidered. Having the same cut off for everyone regardless of age, sex or size completely ignores the fact that heart wall thickness is strongly influenced by these factors.’
The Life-Saving Impact of Precision
The implications of this research are far-reaching. As Dr. Sonya Babu-Narayan, Clinical Director at the British Heart Foundation, notes, ‘Hypertrophic cardiomyopathy is a severe, potentially life-threatening condition, and missed diagnosis means people that might benefit from new and effective treatments could slip through the net.’ With effective HCM treatments now available, accurate diagnosis has never been more crucial.
A New Era of Equitable Care
This study represents a pivotal step towards closing the diagnostic gender gap in heart disease. By embracing a personalized, data-driven approach, we can ensure that no one is left behind due to outdated, biased guidelines. As Dr. Babu-Narayan affirms, ‘Our research provides a long-overdue update, showing that a personalised approach improves the accuracy of diagnosis. Effective treatments for HCM are starting to be used for the first time, making it more important than ever that we can correctly identify those who need them.’















